What is Complex PTSD?
Types of traumas known to causes Complex PTSD include multiple incidents of child abuse, particularly repeated child physical abuse and repeated child sexual abuse, prolonged domestic violence, concentration camp experiences, torture, slavery, and genocide campaigns.[3] Complex Post-traumatic Stress Disorder is a diagnosis in the World Health Organization's ICD-11 diagnostic manual, but is not in the American DSM-5 psychiatric manual (which was last updated in 2013).[3], [5]
Differences between PTSD and Complex PTSD

Disturbances in Self-Organization (DSO)
- affective dysregulation (AD),
- severe and persistent difficulties managing emotions
- negative self-concept (NSC), and
- low self-worth [3], [10]
- disturbances in relationships (DR)
- difficulties in feeling close to people and in sustaining interpersonal relationships
Complex PTSD Symptoms
- Interpersonal problems includes social and interpersonal avoidance (avoiding relationships), feeling distance or cut off from others, and never feeling close to another person.
- Negative self-concept involves feelings of worthlessness and guilt. While survivors of PTSD may feel "not myself", a survivor of Complex PTSD may feel no sense of self at all or experience a changed personality; a few may feel as if they are no longer human at all (Lovelace and McGrady, 1980; Timerman, 1981).[1]:385-386. Believing yourself to be "contaminated, guilty, and evil" is commonly reported by survivors of Complex PTSD. A fragmented identity is common, with Dissociative Identity Disorder occurring in some people. [1]:386
- Interpersonal sensitivity includes having feelings which are easily hurt, anger/temper outbursts and difficulties with interpersonal relationships. Complex PTSD is normally the result of interpersonal trauma, the long duration of the trauma and the control of the perpetrator(s) prevents people from expressing anger or rage at the perpetrator(s) during the trauma; anger and rage both at perpetrators and the self can only be fully expressed after the trauma ends. Prolonged abuse normally leads to a loss of previously-held beliefs, with feelings of "being forsaken by both man and God". [1]:382,386
- Severe and persistent affect dysregulation, which means having great difficulty managing emotions, and is often referred to as "difficulties with emotional regulation". This may result in dissociative symptoms when under stress, and emotional numbing or the inability to experience pleasure. The unexpressed anger and internalized rage resulting from the trauma may lead to self-destructive or reckless/risk taking behaviors, e.g., self-harm and/or suicide attempts, which may be driven by a sense of self-hatred. [1]:382, [3] [6]
- The diagnostic criteria for PTSD must also be met by people with Complex PTSD, these are:
- a persistent sense of threat, e.g. hypervigilance and being easily startled, which may cause a diminished startle response in some people
- avoiding reminders of the traumas,
- and re-experiencing or reliving the traumas, for example flashbacks and intrusive thoughts about the trauma.[3]
Observers who have never experienced prolonged terror, and who have no understanding of coercive methods of control, often presume that they would show greater psychological resistance than the victim in similar circumstances. The survivor's difficulties are all too easily attributed to underlying character problems, even when the trauma is known. When the trauma is kept secret, as is frequently the case in sexual and domestic violence, the survivor's symptoms and behavior may appear quite baffling, not only to lay people but also to mental health professionals. The clinical picture of a person who has been reduced to elemental concerns of survival is still frequently mistaken for a portrait of the survivor's underlying character." [1]:388
Complex PTSD, BPD and Personality Disorders
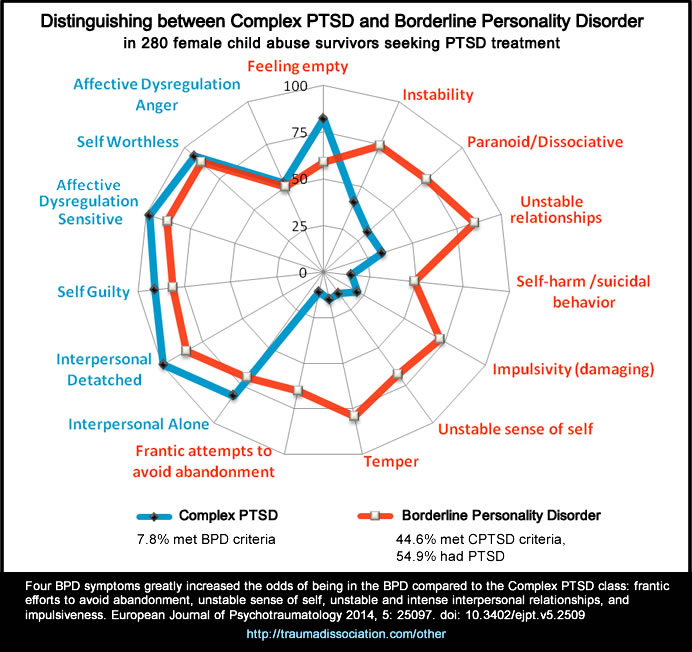
Concepts of personality developed in ordinary circumstances are frequently applied to survivors, without an understanding of the deformations of personality which occur under conditions of coercive control. Thus, patients who suffer from the complex sequelae of chronic #trauma commonly risk being misdiagnosed as having personality disorders. They may be described as "dependent," "masochistic," or "self−defeating." Earlier concepts of masochism or repetition compulsion might be more usefully supplanted by the concept of a complex traumatic syndrome.[1]:388
• See also: Enduring Personality Change After Catastrophic Experience
Complex Post Traumatic Stress Disorder Definition
Complex post traumatic stress disorder
Code 6B41- In addition, Complex PTSD is characterised by severe and persistent
- 1) problems in affect regulation;
- 2) beliefs about oneself as diminished, defeated or worthless, accompanied by feelings of shame, guilt or failure related to the traumatic event; and
- 3) difficulties in sustaining relationships and in feeling close to others.
ICD-11 Diagnostic criteria
Required Features:- • Exposure to an event or series of events of an extremely threatening or horrific nature, most commonly prolonged or repetitive events from which escape is difficult or impossible. Such events include, but are not limited to, torture, concentration camps, slavery, genocide campaigns and other forms of organized violence, prolonged domestic violence, and repeated childhood sexual or physical abuse.
- • Following the traumatic event, the development of all three core elements of Post-Traumatic Stress Disorder, lasting for at least several weeks:
- 1. Re-experiencing the traumatic event after the traumatic event has occurred, in which the event(s) is not just remembered but is experienced as occurring again in the here and now. This typically occurs in the form of vivid intrusive memories or images; flashbacks, which can vary from mild (there is a transient sense of the event occurring again in the present) to severe (there is a complete loss of awareness of present surroundings), or repetitive dreams or nightmares that are thematically related to the traumatic event(s). Re-experiencing is typically accompanied by strong or overwhelming emotions, such as fear or horror, and strong physical sensations. Re-experiencing in the present can also involve feelings of being overwhelmed or immersed in the same intense emotions that were experienced during the traumatic event, without a prominent cognitive aspect, and may occur in response to reminders of the event. Reflecting on or ruminating about the event(s) and remembering the feelings that one experienced at that time are not sufficient to meet the re-experiencing requirement.
- 2. Deliberate avoidance of reminders likely to produce re-experiencing of the traumatic event(s). This may take the form either of active internal avoidance of thoughts and memories related to the event(s), or external avoidance of people, conversations, activities, or situations reminiscent of the event(s). In extreme cases the person may change their environment (e.g., move house or change jobs) to avoid reminders.
- 3. Persistent perceptions of heightened current threat, for example as indicated by hypervigilance or an enhanced startle reaction to stimuli such as unexpected noises.
Hypervigilant persons constantly guard themselves against danger and feel themselves or others close to them to be under immediate threat either in specific situations or more generally. They may adopt new behaviours designed to ensure safety (not sitting with ones’ back to the door, repeated checking in vehicles’ rear-view mirror). In Complex Post-Traumatic Stress Disorder, unlike in Post-Traumatic Stress Disorder, the startle reaction may in some cases be diminished rather than enhanced. - • Severe and pervasive problems in affect regulation.
Examples include heightened emotional reactivity to minor stressors, violent outbursts, reckless or self-destructive behaviour, dissociative symptoms when under stress, and emotional numbing, particularly the inability to experience pleasure or positive emotions. - • Persistent beliefs about oneself as diminished, defeated or worthless, accompanied by deep and pervasive feelings of shame, guilt or failure related to the stressor.
For example, the individual may feel guilty about not having escaped from or succumbing to the adverse circumstance, or not having been able to prevent the suffering of others. - • Persistent difficulties in sustaining relationships and in feeling close to others. The person may consistently avoid, deride or have little interest in relationships and social engagement more generally. Alternatively, there may be occasional intense relationships, but the person has difficulty sustaining them.
- • The disturbance results in significant impairment in personal, family, social, educational, occupational or other important areas of functioning. If functioning is maintained, it is only through significant additional effort.
- • Suicidal ideation and behaviour, substance abuse, depressive symptoms, psychotic symptoms, and somatic complaints may be present.
- The onset of Complex Post-Traumatic Stress Disorder symptoms can occur across the lifespan, typically after exposure to chronic, repeated traumatic events and/or victimization that have continued for a period of months or years at a time.
- Symptoms of Complex Post-Traumatic Stress Disorder are generally more severe and persistent in comparison to Post-Traumatic Stress Disorder.
- Exposure to repeated traumas, especially in early development, is associated with a greater risk of developing Complex Post-Traumatic Stress Disorder rather than Post-Traumatic Stress Disorder
Enduring Personality Change After Catastrophic Experience
The earlier ICD-10 diagnostic manual included a diagnosis of Enduring Personality Change After Catastrophic Experience (EPCACE) in the Disorders of adult personality and behavior section. This is regarded as equivalent to Complex PTSD.[3]
Code F62.0
"Enduring personality change may follow the experience of catastrophic stress. The stress must be so extreme that it is unnecessary to consider personal vulnerability in order to explain its profound effect on the personality. Examples include concentration camp experiences, torture, disasters, prolonged exposure to life-threatening circumstances (e.g. hostage situations - prolonged captivity with an imminent possibility of being killed). Post-traumatic stress disorder (F43.1) may precede this type of personality change, which may then be seen as a chronic, irreversible sequel of stress disorder. In other instances, however, enduring personality change meeting the description given below may develop without an interim phase of a manifest post-traumatic stress disorder.
However, longterm change in personality following short-term exposure to a lifethreatening experience such as a car accident should not be included in this category, since recent research indicates that such a development depends on a pre-existing psychological vulnerability." [2]:163
ICD-10 EPCACE Diagnostic guidelines
The personality change should be enduring and manifest as inflexible and maladaptive features leading to an impairment in interpersonal, social, and occupational functioning. Usually the personality change has to be confirmed by a key informant. In order to make the diagnosis, it is essential to establish the presence of features not previously seen, such as:
- a hostile or mistrustful attitude towards the world;
- social withdrawal;
- feelings of emptiness or hopelessness;
- a chronic feeling of being "on edge", as if constantly threatened
- estrangement.
This personality change must have been present for at least 2 years, and should not be attributable to a pre-existing personality disorder or to a mental disorder other than post-traumatic stress disorder (F43.1).
Includes:- Personality change after concentration camp experiences
- Personality change after disasters,
- Prolonged captivity with an imminent possibility of being killed
- Prolonged exposure to life-threatening situations such as being a victim of terrorism
- Torture
- post-traumatic stress disorder (F43.1) [2]:163-164
- Brain damage or disease which may cause similar clinical features must be ruled out.
Treatment for Complex PTSD
See also Treatment for Complex PTSD

