Maladaptive Daydreaming Scale
What is maladaptive daydreaming?
Maladaptive daydreamers
"spend hours completely absorbed in highly structured and very fanciful daydreams, often often accompanied by stereotypical movements, hindering functioning and participation in everyday life".[2], [4]Maladaptive daydreaming may occur when listening to music, or when pacing, rocking, or making certain hand movements. Ross et al. (2020) states that maladaptive daydreaming is not a variation of normal daydreaming or normal absorption due to:
- obsessive-compulsive aspects, which are not explained by absorption
- the clinically significant levels of distress it causes
- the significant impairment it causes [9]
The 16 item Maladaptive Daydreaming Scale
The maladaptive daydreaming scale has been translated into multiple different languages.[2], [3]
This page is an electronic version of the English MDS-16 self-assessment questionnaire.
Score
| Interpreting scores | |
|---|---|
| 0 to 39 | Normal range, maladaptive daydreaming is unlikely |
| 36.4 | Average score for in-patients with DID in a trauma unit (33 patients, included some maladaptive daydreamers) [9] |
| 40 or above | Probable maladaptive daydreaming [10] |
| 66.91 | average score for probable maladaptive daydreamers in a study of over 500 [20] |
| These scores are for adolescents and adults aged 13 or over.[3], [10] Children may have higher or lower score ranges. A clinical assessment is needed for diagnosis.[3], [4] | |
About Maladaptive Daydreaming Scale scores
This page is for information only and does not provide medical advice. If you score in the high range then a clinical assessment from a trained clinician would still be needed to make a diagnosis; although Maladaptive Daydreaming is not a generally accepted diagnosis, proposed diagnostic criteria have been published.[4]
DID and Maladaptive Daydreaming
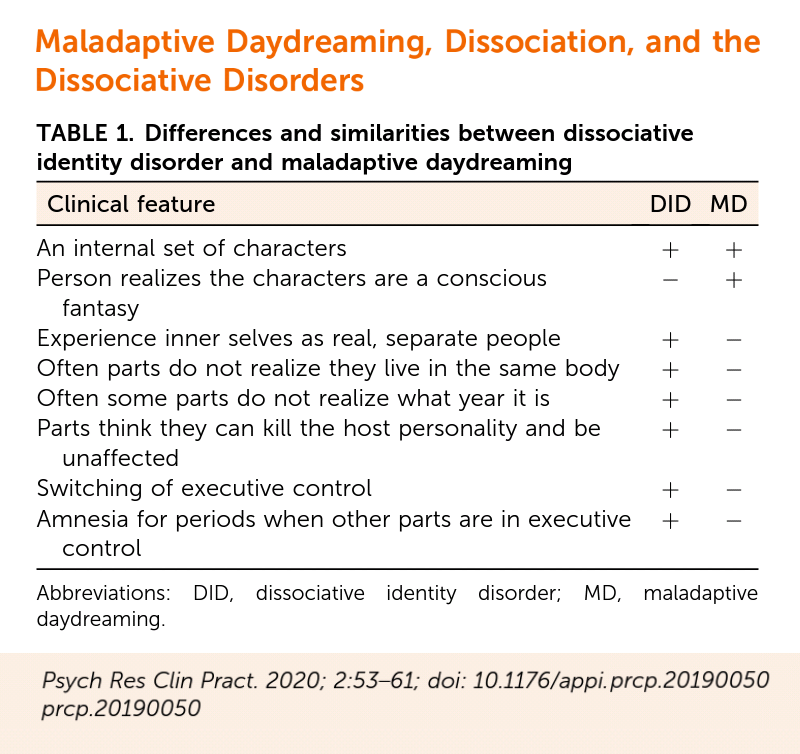
Similarities
Maladaptive Daydreaming may, in some people, be incorrectly self-diagnosed as Other Specified Dissociative Disorder presentation 1 — symptoms similar to Dissociative Identity Disorder but without amnesia —sometimes known as OSDD-1b [13] or
Dissociative Identity Disorder (DID) due to overlapping features which may include:
- a private inner world in which alter personalities (in DID/OSDD) or inner characters (in maladaptive daydreaming) can interact with each other
- a minority of people with DID have "fantastic landscapes" in an inner world, and "inner characters" who do not participate in therapy
- mental detachment in the form of absorption, where there is a lack of awareness of events in the environment because attention is focused inwards
- persistent dissociation that is not limited to absorption, e.g. involving depersonalization and other types of dissociation, and
- a history of childhood emotional abuse is common in both maladaptive daydreaming and DID/OSDD
- a sense of presence of the inner characters in maladaptive daydreaming, which could be confused with an awareness of some of the actions or thoughts of alters in DID (known as co-consciousness or co-presence).[3], [6], [8], [9], [13]
Polyfragmented DID and Maladaptive Daydreaming
A significant minority of people with DID have over 100 alter identities, which is known as polyfragmented DID. Maladaptive daydreamers may also have a large number of inner characters, sometimes hundreds or thousands.[9]Despite the clear differences between the two disorders, some cases of dissociative identity disorder with large numbers of identity states, the complexity and elaboration of the inner characters, and their interactions can resemble those in maladaptive daydreaming —Ross, C.A., Ridgway, J., & George, N. (2020)
Differences from DID/OSDD
Significant differences exist between maladaptive daydreaming and the complex dissociative disorders Dissociative Identity Disorder and Other Specified Dissociative Disorder type 1 [2], [5], [9] which go beyond the differences in the diagnostic criteria, and maladaptive daydreamers present differently to people with DID or OSDD in clinical practice. [13]
Differences between maladaptive daydreaming and DID/OSDD-1 include:
DID or OSDD-1 can only be diagnosed when symptoms cannot be better explained by another psychiatric or medical condition (e.g. maladaptive daydreaming), but a subgroup of people have both maladaptive daydreaming in addition to DID or OSDD.[5], [9]- Daydreaming and dissociative symptoms in DID and OSDD are not triggered, maintained or enhanced when the person makes stereotypical movements such as pacing, in DID and OSDD triggers typically cause flashbacks, identity alteration (switching) or dissociation other than daydreaming [5]
- People without maladaptive daydreaming have no desire for evocative music to "enhance" their daydreaming or dissociation
- People with DID or OSDD do not yearn to spend many hours a day daydreaming or find daydreaming extremely rewarding.[14], [15], [16]
- in DID/OSDD, people have multiple dissociative parts to their personality, which may feel either like different sides or aspects of them (e.g., "me but a different me") or may feel totally different to them (e.g., "not me", like having "multiple personalities" that physically take control of their body), [21] but in maladaptive daydreaming the inner characters and their interactions are purely fantasy, e.g., intricate plots with characters who act out ongoing themes or stories, often with an idealized version of the self or feeling like the narrator [1], [9], [11]
- Unlike DID and OSDD, in maladaptive daydreamers, the inner characters (which they may describe as "personalities" or "alters") never physically take executive control. In DID/OSDD alter personalities are not "inner" characters - they physically take control, alters can talk to other people or engage in self-destructive behaviors causing physical injury such as cutting the person's body.[1], [5], [9]
- Co-morbid Attention-Deficit/Hyperactivity Disorder (ADHD) (especially the inattentive type) is extremely common in maladaptive daydreamers, affecting about 75%,[5] but is far less common in DID/OSDD. Co-morbid Posttraumatic Stress Disorder is uncommon in maladaptive daydreamers, [5] but is extremely common in DID/OSDD. [21]
- A history of childhood physical and sexual abuse is reported by 80-95% of people with DID/OSDD but is significantly less common in maladaptive daydreamers.[5], [9], [19] Maladaptive daydreamers have often experienced a range of adverse childhood experiences, including childhood emotional abuse, physical neglect, witnessing parental violence, and parental separation; only a subgroup are suvivors of childhood physical and sexual abuse.
- Current social isolation is a one of two potential pathways linked to developing maladaptive daydreaming,[11] but is not linked to developing DID/OSDD.[5]
- Co-morbid obsessive-compulsive and related disorders, particularly excoriation disorder and obsessive-compulsive disorder affect over half maladaptive daydreamers, but far less common in people with DID/OSDD.[5], [21]
The Maladaptive Daydreaming Scale (MDS-16) is the primary screening tool developed to assess for Maladaptive Daydreaming, it does not assess dissociative symptoms unrelated to daydreaming.[3], [11]
Structured Clinical Interview for Maladaptive Daydreaming
The Structured Clinical Interview for Maladaptive Daydreaming (SCIMD) was developed in 2017 to diagnose maladaptive daydreaming based on the proposed diagnostic criteria.[4]Further self-assessment measures
The Dissociative Experiences Scale (DES) is a screening tool commonly used to assess if someone is likely to have Dissociative Identity Disorder or similar forms of Other Specified Dissociative Disorder/Partial Dissociative Identity Disorder.
In a study of 100 in-patients at a trauma unit specializing in dissociative disorders, the thirty-three people with DID scored an average of 51.6 on the Dissociative Experiences Scale (and an average of 36.4 on the MDS-16), showing a very high level of dissociation.[9] The study found 49% of patients had maladaptive daydreaming disorder with 23% having unspecified maladaptive daydreaming (subthreshold symptoms), and 89% of the full group had DID or OSDD.[9] However, maladaptive daydreamers were more likely to have ADHD (especially the inattentive type), an anxiety disorder (especially social anxiety or generalized anxiety disorders), depression or an obsessive-compulsive related disorder (particularly excoriation/skin picking or OCD) than a co-morbid dissociative disorder.[5] A relatively small study of 39 maladaptive daydreamers found 12.8% had a co-morbid dissociative disorder (Depersonalization/Derealization Disorder, Dissociative Amnesia or Unspecified Dissociative Disorder), but none had DID or OSDD - however groups of less than 100 are unlikely to be large enough to definitely contain people with DID or OSDD.[5]
Somer et al. 2016's study of 336 adult maladaptive daydreamers found they had an average DES score of 29.79, which is very similar to the DES cut-off score of 30 that indicating a possible dissociative disorder, and very close to the average DES score of 31 found in people with posttraumatic stress disorder - but much lower than is typical for DID. [2], [9], [17] People with Other Specified Dissociative Disorder score an average of 36 on the DES, and people with DID score much higher, averaging 48, although a clinical interview is needed to diagnose. [17]
Somer et al. 2016's study of 336 adult maladaptive daydreamers found they had an average DES score of 29.79, which is very similar to the DES cut-off score of 30 that indicating a possible dissociative disorder, and very close to the average DES score of 31 found in people with posttraumatic stress disorder - but much lower than is typical for DID. [2], [9], [17] People with Other Specified Dissociative Disorder score an average of 36 on the DES, and people with DID score much higher, averaging 48, although a clinical interview is needed to diagnose. [17]
The Creative Experiences Questionnaire (CEQ by Merckelbach et al. 2001, which assesses fantasy-proneness during childhood has been found to show higher scores in maladaptive daydreamers than in people with DID/OSDD or the general population.[2] Maladaptive daydreamers scored an average of 13.75 on the CEQ,[2] but people with DID are no more fantasy-prone than the general population, with Nijenhuis & Reinders (2016) reporting an average CEQ score of 9.83 for people with DID.[14], [18]
The Adverse Childhood Experiences scale (ACE) is a standardized way to measure potentially harmful childhood experiences, including abuse and neglect, which may be useful identifying levels of childhood abuse, maltreatment and adversity; ACE scores are higher in people with DID/OSDD-1 than in maladaptive daydreamers without co-morbid DID or OSDD-1.
Cite this page
Traumadissociation.com . Maladaptive Daydreaming Scale. Retrieved from .The 16 item Maladaptive Daydreaming Scale (MDS-16) including questions, answers and scoring is copyrighted to Eli Somer, Jayne Bigelsen, Jonathan Lehrfeld and Daniela Jopp (2016). It was published with the following copyright information:
"The MDS-16 is an open access measure and is available for research and clinical use without charge. We request that any research paper and publication that will have used the MDS-16 be shared with the ICMDR team, regardless of the language of the manuscript, with the understanding that we might add it to our online repository of MD publications."The remaining information can be copied or modified for any purpose, including commercially, a link back would be appreciated. License: CC BY-SA 4.0
External links
- Translations of the Maladaptive Daydreaaming Scale - available in including Albanian, Arabic, Armenian, Bengali, Bulgarian, Catalan, Chinese, Croatian, Danish, Dutch, Estonian, French, Georgian, German, Greek, Hindi, Hungarian, Hebrew, Italian, Japanese, Korean, Kyrgyz, Lithuanian, Marathi, Mecadonian, Montenegrin, Norwegian, Persian, Polish, Portuguese, Brazilian Portuguese , Romanian, Russian, Slovenian, Turkish, Serbian, Swedish, Spanish, and Vietnamese.
- Maladaptive daydreaming research - The International Consortium for Maladaptive Daydreaming Research
- Structured Clinical Interview for Maladaptive Daydreaming (in Maladaptive Daydreaming: Proposed Diagnostic Criteria and Their Assessment With a Structured Clinical Interview (2017)
- Somer Clinic YouTube channel for DID and Maladaptive Daydreaming
References
- 1. Somer, E. (2002). Maladaptive daydreaming: A qualitative inquiry. Journal of Contemporary Psychotherapy, 32(2), 197–212.
- 2. Somer, E., Lehrfeld J., Jopp, D.S., & Bigelsen, J. (2016). Development and Validation of the Maladaptive Daydreaming Scale (MDS). Consciousness and Cognition, 39, 77–91. doi: 10.1016/j.concog.2015.12.001.
- 3. Somer, E., Bigelsen, J., Lehrfeld J., & Jopp, D.S. (2016). The 16-item Maladaptive Daydreaming Scale (MDS-16).
- 4. Somer, E., Soffer-Dudek, N., Ross, C. A., & Halpern, N. (2017). Maladaptive Daydreaming: Proposed Diagnostic Criteria and Their Assessment With a Structured Clinical Interview. Psychology of Consciousness: Theory, Research, and Practice, 4(2), 176–189.
- 5. Somer, E., Soffer-Dudek, N., & Ross, C. A. (2017). The comorbidity of daydreaming disorder (Maladaptive Daydreaming). Journal of Nervous and Mental Disease, 205(7), 525–530.
- 6. Ross, C. A. (2018). The potential relevance of maladaptive daydreaming in treatment of dissociative identity disorder in persons with ritual abuse and complex inner worlds. Frontiers in the Psychotherapy of Trauma and Dissociation, 2(1), 160–173.
- 7. Somer, E. (2018). Maladaptive daydreaming: Ontological analysis, treatment rationale; a pilot case report. Frontiers in the Psychotherapy of Trauma and Dissociation, 1(2), 1–22.
- 8. Somer, E. (2019). COMMENTARY on dissociative identity disorder and maladaptive daydreaming. Frontiers in the Psychotherapy of Trauma and Dissociation, 3(1), 14–18.
- 9. Ross, C.A., Ridgway, J., & George, N. (2020). Maladaptive daydreaming, dissociation, and the dissociative disorders. Psychiatric Research and Clinical Practice, 2(2), 53–61.
- 10. Soffer-Dudek, N. (2021). [Corrigendum for The MDS-16 (English version) cutoff score]. Unpublished raw data.
- 11. Soffer-Dudek, N., & Somer, E. (2022). Maladaptive daydreaming is a dissociative disorder: Supporting evidence and theory. In Dissociation and the Dissociative Disorders (pp. 547–563). Routledge.
- 12. The International Consortium for Maladaptive Daydreaming Research. Maladaptive daydreaming research.
- 13. Christensen, E. M. (2022). The online community: DID and plurality. European Journal of Trauma & Dissociation, 6(2), 100257.
- 14. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. (5th ed.). Washington, D.C.: American Psychiatric Association. ISBN 0890425558.
- 15. World Health Organization. (2023). Dissociative Identity Disorder. ICD-11 for mortality and morbidity statistics. World Health Organization.
- 16. World Health Organization. (2023). Partial Dissociative Identity Disorder. ICD-11 for mortality and morbidity statistics. World Health Organization.
- 17. Carlson, E.B. & Putnam, F.W. (1993). An update on the Dissociative Experience Scale. Dissociation. 6(1), 16-27. Note: Dissociative Experiences Scale-II included in Appendix.
- 18. Nijenhuis, E.R.S. & Reinders, A.A.T.S. (2016). Fantasy proneness in dissociative identity disorder. PLoS, 7(6), e39279. Supporting Information S1. doi:10.1371/journal.pone.0039279.s001
- 19. Dalenberg, C. J., Brand, B. L., Gleaves, D. H., Dorahy, M. J., Loewenstein, R. J., Cardena, E., ... & Spiegel, D. (2012). Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychological bulletin, 138(3), 550.
- 20. Somer, E., Abu-Rayya, H. M., & Brenner, R. (2021). Childhood Trauma and Maladaptive Daydreaming: Fantasy Functions and Themes In A Multi-Country Sample. Journal of Trauma & Dissociation, 22(3), 288-303.
- 21. International Society for the Study of Trauma and Dissociation. (2011). Guidelines For Treating Dissociative Identity Disorder In Adults, Third Revision: Summary Version. Journal of Trauma & Dissociation,12(2), 188-212. doi: 10.1080/15299732.2011.537248.

